Blog
Learn something good today!
Your guide to medicinal wellness
The Hidden Impact of Processed Food and Sugary Drinks on Liver Health
In today’s fast-paced world, convenience often comes at a cost especially when it comes to our health. Processed foods and sugary drinks have become dietary staples for many, but their long-term effects on the liver are often overlooked. The liver, a vital organ responsible for detoxifying the body, metabolizing nutrients, and regulating blood sugar, bears the brunt of our modern eating habits. Over time, poor dietary choices can significantly impair liver function and increase the risk of liver-related diseases.
Liver’s Role in Digestion and Metabolism
The liver plays a central role in breaking down food and regulating substances in the blood. It processes carbohydrates, fats, and proteins, stores vitamins and minerals, and removes toxins. When you consume food and beverages, the liver filters out harmful substances and converts excess nutrients into forms the body can use or store. However, this system can be overwhelmed by constant exposure to unhealthy ingredients, especially those found in processed items and sugar-laden drinks.
The Risk of Non-Alcoholic Fatty Liver Disease (NAFLD)
One of the most serious consequences of overconsuming processed food and sugary drinks is the development of non-alcoholic fatty liver disease (NAFLD). This condition occurs when fat builds up in the liver due to causes unrelated to alcohol consumption. Foods high in refined sugars and unhealthy fats, such as packaged snacks, sugary cereals, soft drinks, and fast food, contribute directly to this accumulation.
Fructose, a type of sugar commonly found in sweetened beverages and processed foods, is particularly harmful. Unlike glucose, which is used by many cells in the body, fructose is metabolized almost exclusively by the liver. When consumed in excess, it leads to the creation of fat within liver cells—a process that can trigger inflammation, liver scarring, and eventually more serious conditions like cirrhosis or liver failure.
Inflammation and Oxidative Stress
Beyond fat accumulation, processed foods and sugary drinks can also promote chronic inflammation and oxidative stress. These reactions occur when the liver is repeatedly exposed to artificial additives, trans fats, and high sugar content. Inflammatory signals disrupt the liver’s normal repair processes and increase the risk of liver cell damage. Over time, these effects can diminish liver function and contribute to the progression of liver disease.
Oxidative stress, caused by an imbalance between free radicals and antioxidants in the body, further damages liver cells and impairs their ability to regenerate. Many processed foods are low in natural antioxidants, making it even harder for the liver to defend itself against the damage.
Insulin Resistance and Metabolic Dysfunction
Another major consequence of consuming excessive sugar and processed food is the development of insulin resistance. This condition occurs when the body’s cells stop responding properly to insulin, leading to elevated blood sugar levels and increased fat storage. The liver plays a key role in managing glucose, and insulin resistance can disrupt this balance, increasing the liver’s fat content and worsening NAFLD.
Processed foods are often high in simple carbohydrates and low in fiber, which causes spikes in blood sugar and insulin. Over time, this pattern contributes to metabolic syndrome, a cluster of conditions including obesity, high blood pressure, and abnormal cholesterol levels all of which strain liver function and increase the risk of liver-related complications.
Conclusion
The effects of processed foods and sugary drinks extend far beyond weight gain or dental health—they strike at the core of the body’s metabolic powerhouse, the liver. By understanding the role the liver plays in maintaining overall health, we can make more informed food choices that protect this essential organ. In a world full of quick meals and tempting treats, prioritizing liver-friendly nutrition is an investment in long-term vitality and disease prevention.
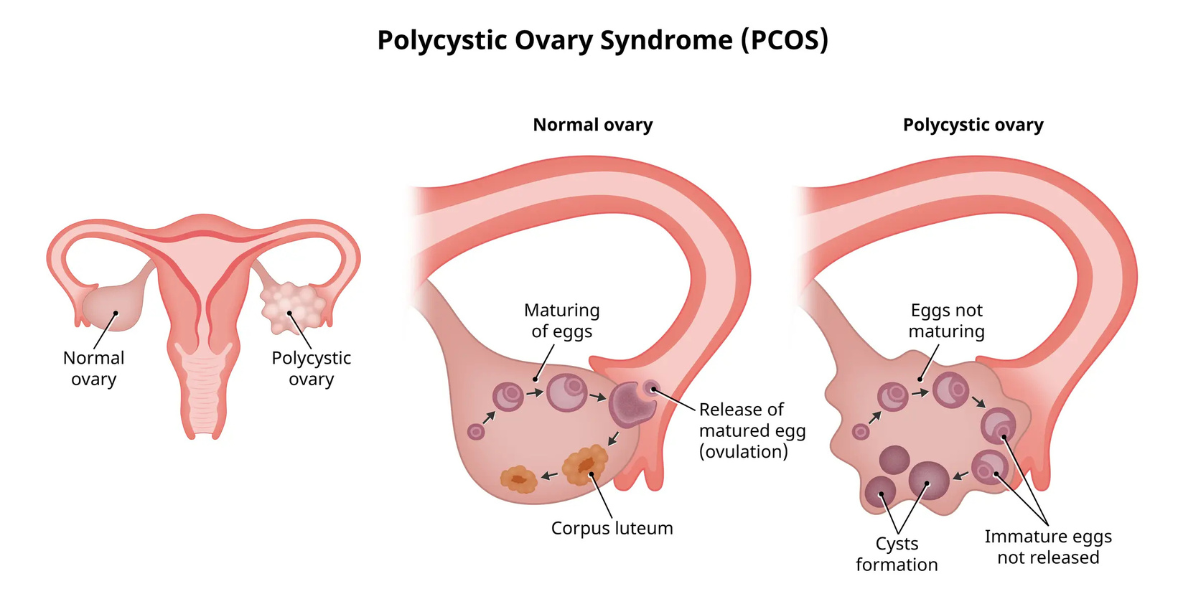
How to Deal with Stress-Induced PCOS Flare-Ups
Polycystic Ovary Syndrome (PCOS) is a hormonal condition that affects millions of women worldwide, often causing irregular periods, weight gain, acne, and fertility issues. While its causes are multifactorial ranging from genetics to insulin resistance, one often underestimated trigger is stress. Emotional and physical stress can act as a powerful disruptor of hormonal balance, exacerbating PCOS symptoms or even triggering flare-ups. Understanding the link between stress and PCOS is the first step in managing its effects.
The Stress-PCOS Connection
Stress impacts the body in numerous ways, but for women with PCOS, it can wreak particular havoc on hormone levels. When you’re under stress, your body produces more cortisol - the stress hormone. Elevated cortisol can interfere with insulin regulation and androgen levels, both of which are already problematic in PCOS. This hormonal imbalance can worsen symptoms such as irregular cycles, increased facial hair, acne, and even weight gain. Moreover, stress can lead to poor sleep and unhealthy eating habits, creating a cycle that makes PCOS harder to manage.
Recognizing the Triggers
Not all stress is obvious. Daily pressures like deadlines, relationship tensions, lack of sleep, or even excessive exercise can silently raise stress levels. For women with PCOS, being attuned to these subtle stressors is crucial. Stress-induced flare-ups may show up as delayed periods, more severe cramps, sudden breakouts, or intensified fatigue. Recognizing when these symptoms align with periods of stress can help in taking timely steps to prevent a downward spiral.
Creating a Calmer Routine
One of the most effective ways to manage stress-induced PCOS symptoms is to establish a consistent, calming daily routine. This includes prioritizing quality sleep, which allows the body to reset hormone levels. Eating at regular intervals and choosing a balanced diet rich in fiber, lean proteins, and healthy fats can help stabilize blood sugar levels and reduce cortisol spikes. Gentle physical activities like walking, yoga, or stretching can be particularly beneficial not just for physical health but for releasing tension and improving mood.
Emotional Health and Support Systems
Mental and emotional health play a central role in managing PCOS. Cognitive behavioral therapy (CBT), journaling, or even talking to a therapist can provide tools to navigate stress more effectively. For many women, joining a support group of others with PCOS offers not just emotional validation but also shared tips and encouragement. Social connection can significantly lower perceived stress levels and help create a more positive outlook on managing the condition
Conclusion
Living with PCOS is a multifaceted journey, and stress can be a powerful influencer of how symptoms manifest and progress. Through mindful routines, emotional support, and integrated medical care, it’s possible to regain balance even during life’s most stressful moments. Taking care of your stress is not just self-care, it’s an essential part of managing PCOS.
How Posture Affects Your Joint Health
Posture is often seen as a matter of appearance - standing tall and straight versus slouching. But good posture goes far beyond aesthetics, it plays a crucial role in maintaining joint health. Your joints are the connections between bones that allow movement, and they are supported by muscles, ligaments, and tendons. When posture is poor, it can cause misalignment, increase strain, and accelerate wear and tear on these vital structures.
The Link Between Posture and Joint Alignment
Every time you sit, stand, or move, your body relies on proper alignment to distribute weight evenly. When you maintain good posture, your head, shoulders, spine, hips, knees, and ankles line up in a way that keeps pressure off your joints. However, slouching or maintaining awkward positions—like craning your neck toward a screen or standing with your weight on one leg—throws off this alignment. This uneven load increases stress on certain joints, particularly in the neck, shoulders, spine, hips, and knees, which over time can lead to pain, stiffness, and even long-term damage.
Posture and Joint Wear Over Time
Poor posture doesn’t just affect your joints temporarily, it has cumulative effects. When joints are consistently under strain, the cartilage that cushions them may wear down faster, potentially leading to conditions like osteoarthritis. For example, forward head posture can contribute to cervical spine compression, while slouching can put excessive pressure on the lumbar spine and hips. Over time, these repeated stresses can cause inflammation and reduce the range of motion in affected joints.
Impact on Movement and Flexibility
Joint health is closely tied to mobility. Poor posture limits the full range of movement that joints are capable of, and muscles around those joints often become tight or weak from disuse. This imbalance can affect your gait, coordination, and the ease with which you perform everyday tasks. For instance, someone with rounded shoulders may have limited shoulder joint function, making it harder to lift objects or reach overhead. Gradually, these restrictions can turn into chronic discomfort and reduce your overall quality of life.
Preventing Joint Problems Through Better Posture
Improving posture is a preventive step toward protecting your joints in the long term. Simple changes such as adjusting your workstation ergonomics, being mindful of your sitting and standing habits, and incorporating regular stretching or strengthening exercises can help restore alignment. Practices like yoga or Pilates are particularly effective, as they emphasize core strength and body awareness, which support joint stability.
Conclusion
The way you carry yourself each day has a powerful impact on your joint health. While poor posture might seem harmless in the short term, it can silently strain joints and lead to chronic issues over time. By becoming more mindful of your posture and making gradual improvements, you can protect your joints, enhance your mobility, and support your overall musculoskeletal health. Your body’s alignment matters not just for how you look, but for how well you move and feel throughout your life.
The Science Behind Nerve Repair
The human nervous system is an intricate network of electrical highways that control everything from muscle movement to sensory perception and even internal organ function. When a nerve is damaged whether by injury, illness, or chronic condition, it disrupts communication within the body, often resulting in pain or loss of function. However, unlike some tissues that regenerate easily, nerve repair is a complex and delicate process.
Types of Nerve Damage and Their Impact
Nerves can be damaged in several ways. Physical trauma, such as cuts or crushing injuries, can sever or compress nerves. Medical conditions like diabetes, multiple sclerosis, or autoimmune diseases can damage nerves internally through inflammation or poor blood flow. The severity of the damage determines the healing potential. In general, peripheral nerves, the ones outside the brain and spinal cord have a better capacity to heal than central nervous system nerves, which include the brain and spinal cord.
The Role of the Nerve Cells
Nerve cells, or neurons, are composed of a cell body, dendrites (which receive signals), and axons (which transmit them). In many cases of nerve injury, it’s the axon that gets damaged. If the neuron’s cell body remains intact and the surrounding environment is favorable, the axon can begin to regenerate. This process starts with the degeneration of the damaged portion, followed by a slow but determined attempt by the nerve to regrow along its original path. Schwann cells—specialized cells in the peripheral nervous system—play a vital role by cleaning up debris and creating a guiding structure called the “regeneration tube” to help direct axon growth.
The Challenges of Regeneration
Nerve regeneration is a slow process, often progressing at a rate of about 1 millimeter per day. This means recovery from nerve injury can take weeks to months, depending on the location and extent of the damage. During this time, several challenges can arise. Scar tissue, poor blood supply, or ongoing inflammation can interfere with regrowth. Moreover, in the central nervous system, the lack of supportive cells like Schwann cells and the presence of growth-inhibiting molecules make regeneration far more difficult.
Supporting Natural Recovery
While some cases require medical intervention, the body has its own strategies for healing nerves. Good nutrition, physical therapy, and controlling underlying conditions like diabetes are crucial for supporting nerve health. Anti-inflammatory diets, adequate hydration, and specific vitamins particularly B vitamins and antioxidants can contribute to a more favorable environment for nerve repair. Importantly, rest and gradual, guided rehabilitation allow the body time to rebuild connections and regain strength.
Conclusion
Nerve repair is a testament to the body’s resilience and complexity. Though it’s often slow and unpredictable, it reflects a remarkable biological process that combines cellular activity, immune support, and structural regeneration. With the help of medical science and holistic care, many people with nerve damage can experience meaningful recovery. As our understanding of neural regeneration continues to evolve, the future holds even greater promise for restoring the delicate balance of the body’s electrical system.
