What Causes Pain After Shingles?
Shingles is a painful, blistering skin rash caused by the reactivation of the varicella-zoster virus, the same virus that causes chickenpox. While the rash and blisters from shingles usually clear up within a few weeks, some people continue to experience pain long after the skin has healed. This lingering pain can be frustrating and it is most often due to a condition known as postherpetic neuralgia (PHN).
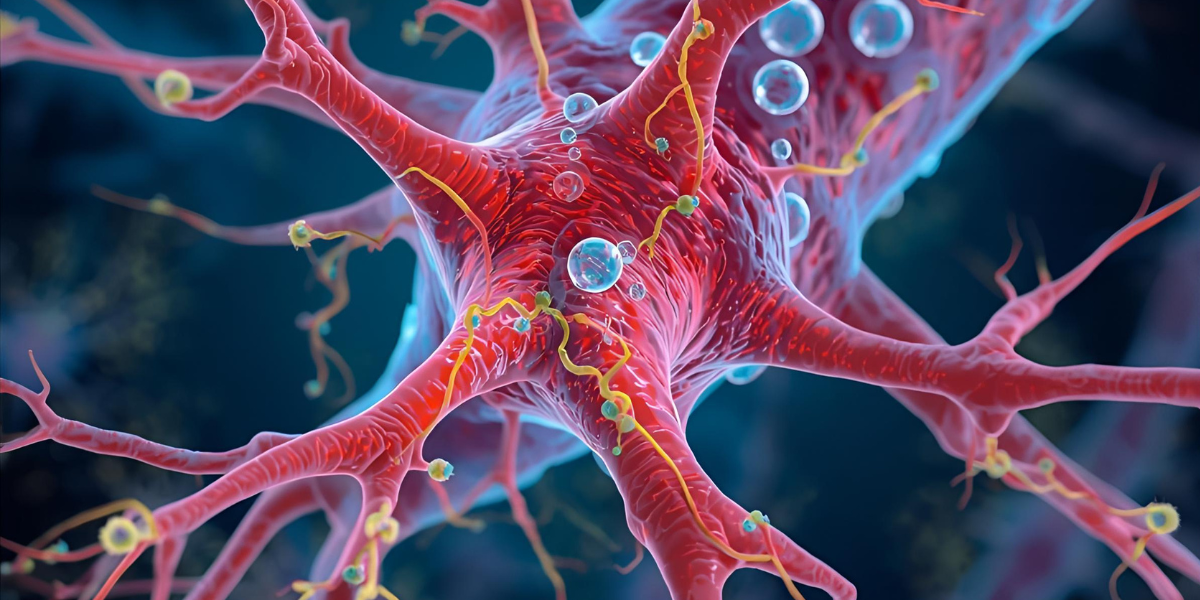
Link Between Shingles and Nerve Pain
Shingles affects the nerves because the varicella-zoster virus lies dormant in nerve tissues after a person recovers from chickenpox. When the virus reactivates, it travels along the nerves to the skin, causing the characteristic shingles rash. In some cases, especially in older adults or people with weakened immune systems, the nerve fibers become damaged during this process. Once the skin heals, the damaged nerves may continue to send pain signals to the brain, even when there’s no longer a visible rash or inflammation. This is what leads to the persistent pain after shingles.
About Postherpetic Neuralgia
Postherpetic neuralgia is the most common complication of shingles and is the medical term for pain that lasts more than three months after the rash has healed. The pain can vary from a constant burning or aching sensation to sharp, stabbing discomfort. Some people may also experience sensitivity to touch, even from clothing or a breeze. The pain is typically located in the same area where the shingles rash originally appeared, most often on one side of the torso, face, or neck.
The risk of developing postherpetic neuralgia increases with age, particularly in individuals over 60. It is also more likely to occur in those who had severe pain or a widespread rash during the acute phase of shingles. While not everyone who gets shingles develops this lingering pain, for those who do, it can significantly affect quality of life.
Why the Pain Persists
The reason postherpetic neuralgia causes such persistent discomfort lies in the nervous system itself. When the virus damages the nerve fibers, those nerves may misfire and send exaggerated pain signals to the brain. In some cases, the brain may interpret normal sensations—like a touch or change in temperature—as painful. Because nerve tissues don’t heal as quickly or completely as other tissues in the body, the pain can linger for months or even years in some individuals.
Moreover, the central nervous system can become “trained” to respond abnormally after long exposure to pain, a phenomenon known as central sensitization. This makes the nerves even more sensitive and reactive, perpetuating the cycle of chronic pain.
Managing Pain After Shingles
Managing post-shingles pain often requires a combination of approaches. Antiviral medications given during the initial outbreak can help reduce the severity of the rash and may lower the risk of developing postherpetic neuralgia. If pain persists, treatments may include nerve pain medications, antidepressants, topical creams, and in some cases, nerve blocks or other procedures.
Preventive measures also play a crucial role. The shingles vaccine significantly reduces the risk of developing shingles and the chance of postherpetic neuralgia if shingles does occur. It is especially recommended for older adults who are at higher risk of complications.
Conclusion
Pain after shingles, particularly postherpetic neuralgia, is a result of nerve damage caused by the varicella-zoster virus. Though the rash may heal, the pain can linger due to ongoing miscommunication between damaged nerves and the brain. Understanding this connection can help patients seek timely treatment and manage symptoms more effectively. As always, prevention through vaccination remains one of the most powerful tools in reducing the burden of this painful condition.