Blog
Learn something good today!
Your guide to medicinal wellness

Practical Tips on Dealing with Night Sweats and Hot Flashes
Hot flashes and night sweats are among the most common and frustrating symptoms many women face during menopause. They can disrupt sleep, affect mood, and make everyday activities uncomfortable. While these symptoms are a natural part of hormonal changes, there are practical ways to manage them and regain a sense of control over your comfort and routine.
Creating a Cooler Sleep Environment
Since night sweats often strike when you’re trying to sleep, adjusting your bedroom environment can make a noticeable difference. Keeping the room temperature slightly cooler than usual and using a fan or air conditioner can also create a more comfortable sleeping space. It’s helpful to avoid heavy blankets or sleeping in layers, and instead opt for light, loose clothing that allows your skin to breathe throughout the night.
Managing Triggers Through Lifestyle Changes
Certain habits and foods can trigger or worsen hot flashes and night sweats. Spicy foods, caffeine, and alcohol are known to raise body temperature and can increase the likelihood of these episodes. Paying attention to when and how often symptoms occur can help you identify patterns and avoid common triggers. Staying hydrated with cool water throughout the day supports temperature regulation and may ease sudden heat episodes. Additionally, practicing relaxation techniques such as deep breathing, meditation, or gentle stretching in the evening can help calm your body and potentially reduce the frequency of nighttime sweating.
Choosing the Right Clothing and Fabrics
What you wear during the day and to bed can influence how your body handles temperature changes. Light, breathable fabrics like cotton and linen are better choices compared to synthetic materials, which tend to trap heat and moisture. Dressing in layers during the day makes it easier to quickly adjust to body temperature shifts caused by a hot flash. At night, opting for moisture-wicking sleepwear can help keep you dry and cool when your body heats up unexpectedly.
Incorporating Physical Activity
Regular physical activity has been shown to help balance hormones and reduce the severity of menopause symptoms, including hot flashes and night sweats. While high-intensity workouts might be uncomfortable during an episode, gentle exercises such as walking, yoga, or swimming can improve circulation and regulate body temperature over time. Exercising earlier in the day is often better, as intense evening workouts may increase body temperature and disrupt sleep.
Practicing Stress Management
Stress can worsen menopausal symptoms, especially hot flashes, by raising your core body temperature and triggering hormonal responses. Developing habits that lower daily stress levels can have a calming effect on both the body and mind. Techniques like mindfulness, journaling, deep breathing, or spending time in nature can be beneficial. Even dedicating a few minutes each day to quiet, peaceful activities can help lessen the intensity of heat episodes.
Conclusion
Though hot flashes and night sweats can be uncomfortable and disruptive, simple adjustments can make them more manageable. Every woman’s experience with menopause is different, so it’s important to find what works best for you. With mindful, practical steps, it’s possible to ease these symptoms and maintain a sense of well-being through this transitional phase.

Is There a Male Biological Clock?
When we hear the phrase “biological clock,” it’s usually in reference to women and the age-related decline in fertility. But what about men? Is there a male biological clock, and does age affect male fertility in the same way? While men can remain fertile longer than women, recent research shows that age does impact male fertility—just differently. Here’s a closer look at the male biological clock and what it means for reproductive health.
Do Men Have a Biological Clock?
Yes, but it ticks a little differently. Unlike women, who are born with a fixed number of eggs, men continue to produce sperm throughout their lives. This means they don’t face a strict “fertility cut-off” like women do after menopause. However, sperm quality does decline with age, and that decline can affect the chances of conception, the time it takes to get pregnant, and even the health of the baby.
How Age Affects Male Fertility
After the age of 35–40, men may experience lower sperm count, reduced sperm motility, increased DNA fragmentation in sperm and abnormal sperm morphology. These changes don’t necessarily make conception impossible, but they can make it harder and may increase the risk of complications.
Studies show that men over 40 are more likely to take longer to conceive, even if their partner is younger and fertile. This is partly due to the decline in sperm quality. As men age, the number of mutations in sperm DNA increases. While most are harmless, some may raise the risk of conditions like autism, schizophrenia, and certain rare genetic syndromes in offspring.
Older paternal age has also been linked to higher risk of miscarriage, lower birth weight in babies and increased risk of stillbirth in some studies
How Late Is Too Late?
There’s no official “expiration date” on male fertility, and many men have fathered healthy children well into their 50s, 60s, and beyond. But from a biological perspective, male fertility begins to decline subtly around age 35 and more significantly after 40–45.
While you can’t stop aging, you can take proactive steps to protect your fertility like staying healthy and avoiding harmful habits. If fatherhood may be far down the line, sperm banking is a safe and effective option.
Conclusion
Yes, men do have a biological clock, though it ticks more slowly and subtly than women’s. Age-related changes in sperm can affect fertility, the health of the pregnancy, and even the baby’s long-term health. The good news? With healthy habits and timely planning, men can support their fertility well into midlife and beyond. It’s never too early or too late to take reproductive health seriously.
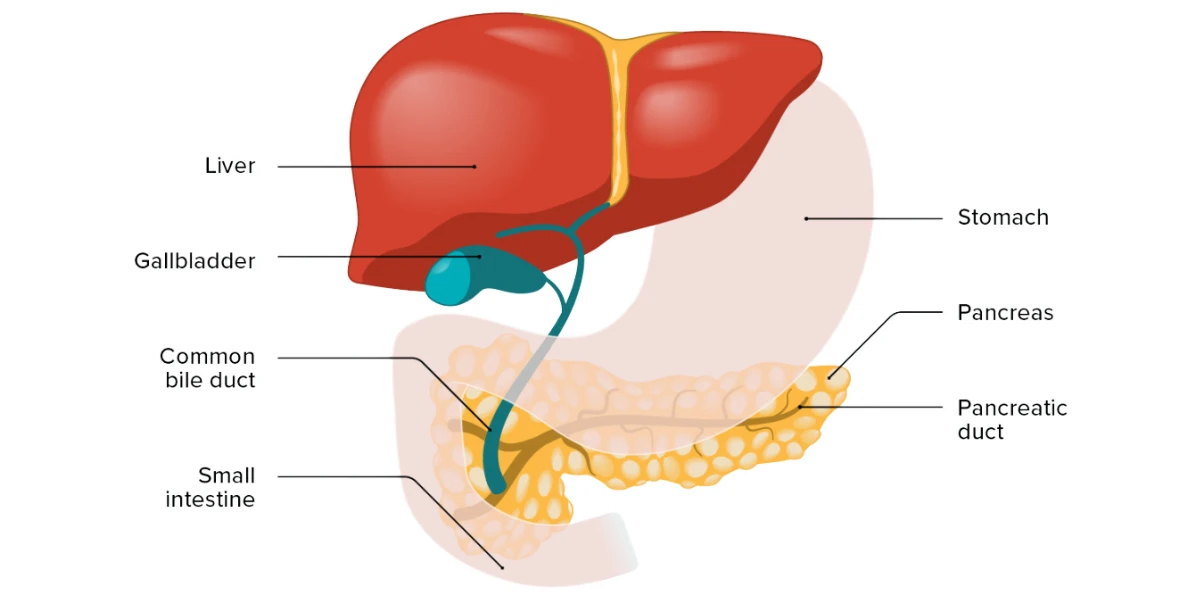
Everyday Habits That Could Be Harming Your Liver
Your liver is one of the most hardworking organs in your body. It filters toxins, aids digestion, stores energy, and plays a vital role in keeping you healthy. But while you may not realize it, some of your daily habits could be putting unnecessary strain on your liver over time. Let’s look at a few lifestyle patterns that might be silently affecting your liver health without you even knowing it.
Excessive Sugar Intake
Sugar isn’t just a problem for your waistline, it can be harmful to your liver too. High consumption of added sugars, especially in processed foods, soft drinks, desserts, and packaged snacks, leads to fat buildup in the liver. Over time, this can result in non-alcoholic fatty liver disease (NAFLD), a growing health issue worldwide. The liver processes excess sugar by turning it into fat, and too much fat stored in the liver can cause inflammation, scarring, and long-term damage. Being mindful of hidden sugars in everyday foods is an important step toward protecting your liver.
Overuse of Painkillers
While popping an over-the-counter painkiller for a headache or backache seems harmless, frequent or excessive use can have serious consequences for your liver. Medications like paracetamol are safe in recommended doses but can become toxic if taken too often or in higher quantities than advised. Since the liver is responsible for breaking down these drugs, overloading it with medication increases the risk of liver damage. Always follow dosage instructions carefully and avoid combining multiple medicines that might contain the same ingredients.
Sedentary Lifestyle
A lack of regular physical activity can indirectly harm your liver. A sedentary lifestyle contributes to weight gain, insulin resistance, and an increased risk of developing fatty liver disease. Regular exercise not only helps maintain a healthy weight but also improves insulin sensitivity and reduces fat deposits in the liver. Even simple activities like walking, stretching, or light workouts can make a big difference over time in keeping your liver functioning well.
Unhealthy Eating Patterns
Skipping meals, overeating, or relying heavily on processed and fried foods can gradually weaken liver function. A diet high in saturated fats, refined carbohydrates, and salty snacks can lead to fat accumulation in the liver. These unhealthy eating habits can trigger inflammation and increase the chances of liver problems over the years. Balancing your meals with fresh fruits, vegetables, whole grains, lean proteins, and healthy fats supports liver health and overall well-being.
Excessive Alcohol Consumption
While occasional, moderate drinking may not cause harm for most people, regularly consuming large amounts of alcohol can severely damage the liver. The liver prioritizes breaking down alcohol over other functions, which can lead to fat buildup, inflammation, and scarring. Over time, this can progress to conditions like alcoholic hepatitis or cirrhosis. Limiting alcohol intake, or avoiding it altogether, gives your liver a much-needed break and helps maintain its natural detoxifying abilities.
Lack of Hydration
Water plays a crucial role in supporting liver function by helping to flush out toxins and waste from the body. When you’re not drinking enough water, your liver has to work harder to process and eliminate waste, which can eventually slow it down. Staying well-hydrated supports digestion, blood circulation, and the liver’s detoxification processes, all of which are essential for keeping your liver healthy and active.
Conclusion
Many everyday habits, even those that seem harmless, can slowly wear down your liver’s ability to function optimally. Being aware of how your lifestyle choices affect this vital organ can help you make smarter, healthier decisions moving forward. Small, consistent changes can go a long way in protecting your liver and ensuring it continues to support you for years to come.

Why a Lot of Adults Experience Arthritis
Arthritis is often thought of as a disease of old age, but many adults begin to feel its effects far earlier than expected. From stiffness in the knees after waking up to persistent joint pain that disrupts daily life, arthritis has become increasingly common among adults of all ages.
Understanding Arthritis and Its Many Forms
Arthritis isn’t a single disease but a term used to describe inflammation of the joints. It encompasses more than 100 different conditions, with osteoarthritis and rheumatoid arthritis being the most common. Osteoarthritis is a degenerative condition that occurs when the cartilage cushioning the joints wears away over time. Rheumatoid arthritis, on the other hand, is an autoimmune disorder where the body’s immune system mistakenly attacks the joint linings. Both lead to pain, swelling, reduced mobility, and joint damage if left untreated.
The Role of Age and Wear and Tear
One of the primary reasons arthritis becomes more prevalent with age is simple wear and tear. As people get older, the cartilage that cushions their joints naturally begins to thin and lose its elasticity. Years of repetitive movements like walking, lifting, typing, or even just standing add up, gradually stressing the joints and accelerating cartilage breakdown. While this process is natural, it affects people differently based on their lifestyle, genetics, and overall health.
Lifestyle Factors That Accelerate Joint Damage
Modern lifestyles play a significant role in the rising incidence of arthritis among adults. Sedentary habits, poor posture, and obesity are major contributors. Excess weight, for example, puts more pressure on weight-bearing joints like the knees, hips, and lower back, speeding up joint degeneration. Meanwhile, a lack of regular physical activity can weaken the muscles that support joints, leading to instability and increased strain. Even occupations that involve repetitive joint movement or heavy lifting can increase arthritis risk over time.
The Influence of Genetics and Family History
Genetics can also influence who gets arthritis. People with a family history of osteoarthritis or autoimmune conditions like rheumatoid arthritis may be more likely to develop symptoms themselves. Certain inherited traits can affect how cartilage is formed or how the immune system behaves, making some individuals more susceptible to early-onset arthritis. While genes cannot be changed, understanding one’s risk can help in taking early preventative steps.
Injuries and Joint Trauma
Injuries sustained during youth or adulthood, especially those involving joints, can set the stage for arthritis later on. Damage to the cartilage, ligaments, or bones around a joint can cause long-term instability or inflammation. Conditions like sports injuries, fractures, or even surgery on a joint may lead to a form of arthritis known as post-traumatic arthritis, which often appears years after the initial injury.
The Importance of Early Recognition and Care
One of the challenges with arthritis is that its early symptoms are often subtle and easy to ignore. Mild stiffness, occasional swelling, or joint discomfort might be dismissed as temporary issues. However, catching arthritis in its early stages can make a big difference. Lifestyle modifications, physical therapy, medication, and other interventions can help manage symptoms and slow disease progression, preserving joint function for longer.
Conclusion
Many adults experience arthritis not just because of aging, but due to a combination of factors including lifestyle, genetics, injuries, and chronic stress on the joints. As people live longer and more sedentary lifestyles become the norm, arthritis has become a common companion in adulthood. Recognizing the early signs and understanding what contributes to joint damage, individuals can take proactive steps to protect their joints, stay mobile, and reduce the impact of arthritis on their lives.
